While much of sports acupuncture today focuses on the treatment of injury (pain relief and restoration of strength), there is a much larger field that acupuncturists are uniquely qualified to treat, yet often skip over: post-exercise recovery.
Recovery is a vital component of an overall exercise or training program. It’s essential for high-level performance and continued athletic improvement. With the appropriate recovery treatments–including acupuncture–athletes can achieve higher training volumes and intensities while avoiding many of the detrimental side-effects of overtraining.
Purpose
This essay aims to present and analyze the research and perspectives on the complex topic of post-exercise recovery and the role of sports acupuncture therein.
Primarily, it will look at the parasympathetic system, how it affects recovery, and how it is stimulated by acupuncture practices.
It will also address the physiology of the time period immediately after exercise as an important biological phenomenon that acupuncturists can use to the advantage of their clients.
Finally, this essay aims to show that sports acupuncture professionals can and should play a larger role in helping athletes recover after exercise.
What is Recovery?
Defining exercise recovery is a challenging task: there are many varied definitions of “recovery”. In the sports acupuncture world, the two most common definitions or views of recovery are as follows:
- As a distinct period of time. Recovery can refer to a specific time frame. This period of time can range from minutes, as in the case of the heart rate returning to near-resting levels, to weeks, as in the return of strength after muscle-damaging exercise.These time frames also vary from person to person. For example, a trained athlete will display a different recovery timeline from that of a healthy individual. Both of these individuals will display vastly different recovery timelines than that of a person who is chronically ill.
- As a physiological state or process. “Recovery” can also refer to a certain set of physiological processes or states which are distinct from resting physiological states and from the physiological state of exercise.This view of exercise recovery is usually localized: it assesses whether the muscles are ready to perform on the day of an event, or if they are weakened or injured.
Within these two definitions of recovery, treatment strategies tend to focus on symptoms of exercise-induced muscle damage and mainly work to blunt the inflammatory responses associated with muscle injury.
Treatments that are based on these perspectives of recovery typically aim to hasten regenerative processes of the muscles with limited consideration for other mechanisms (Minett and Duffield, 2014). This may be through lifestyle (active recovery, sleep), physiological treatment (post-exercise cooling, massage, compression), or nutritional and pharmacological interventions (supplements, anti-inflammatory medications).
These perspectives of recovery are too narrow, and they exclude factors such as illness, sleep, and psychology. These each have a significant impact on recovery and must be managed, in conjunction with the methods described above, in order to allow better performance and reduce the risk of injury.
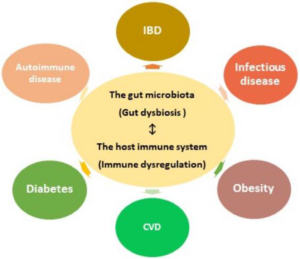
Evidence for Expanding the Definition of Recovery
Various studies have found that single session of intense exercise and prolonged heavy training negatively influences the immune system function (Pedersen, 1998). This was done primarily by measuring SIgA levels, with SIgA being the predominant immunoglobulin found in the saliva other mucosal fluids. It neutralizes toxins and viruses and inhibits the attachment and replication of pathogens (Gleeson et al., 1999).
These studies have demonstrated that (Mackinnon et al., 1993):
- Frequent upper respiratory tract infections (URTI) in elite athletes result in suppression of salivary secretory immunoglobulin A (SIgA) levels.
- The exercise-induced decrease of salivary SIgA was inhibited in the acupuncture treatment group during a competition period.
- The data suggests that acupuncture treatment enhances SIgA secretion in the saliva during the period of continuous physical exercise.
- Therefore, it is possible that the increased risk of URTI in athletes during the competition period is due to a decrease in SIgA levels.
- Acupuncture treatments could reduce the likelihood of infection in athletes and maintain their physical wellbeing by improving levels of SIgA and immunogenic actions.
Sympathetic vs. Parasympathetic Involvement in Exercise Recovery
The human body is intelligently balanced with a complex, built-in network for adapting to stress. This network is known as the autonomic nervous system, and it is comprised of two unique subsystems: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS).
The parasympathetic and sympathetic nervous systems both deal with metabolism, which is a biochemical process within the body that allows healing, growth and adaptation. Metabolism is the pattern of building up and breaking down resources within the body, and can be divided into catabolic and anabolic processes.
The SNS is catabolic, meaning it breaks down resources, usually creating energy that is easily accessible. It mobilizes the these vital resources to help the body defend itself when it’s in danger. The sympathetic nervous system is what sends you into “fight or flight” mode in threatening situations. This system is upregulated during workouts, but ideally, the body only uses the SNS to its full capacity in life-threatening emergencies.
The PNS is anabolic, meaning it builds up resources within the body, usually requiring energy to perform. The parasympathetic nervous system allows the body the resources it needs to adapt and recover. It helps the body to rest, digest, and recover after workouts and strenuous activity. A well-balanced nervous system spends most of its time on parasympathetic activities. An active PNS helps muscle soreness and swelling subside more quickly.
Athletes are vulnerable to becoming SNS-dominant because they experience increased physical stress on a routine basis. By spending more time on sympathetic activities–and, therefore, less time on parasympathetic activities–an athlete’s nervous system will have a harder time helping the body recover.
In addition to the physical stress athletes experience regularly, emotional/mental stress can also play a role in an athlete becoming SNS-dominant. The following stressors can put an additional burden on an athlete’s nervous system:
- Stress at home or at work;
- An upcoming event or season that requires increased training intensity and/or frequency;
- Nervousness or anxiety about an upcoming event or season;
- Acute or chronic psychological disturbances including depression or anxiety;
- Physical illness, either transient or chronic; and/or
- Restricted caloric intake due to an upcoming weigh-in or their sport having another weight component (i.e. wrestling or ballet).
Most athletes will fall into at least one of the above categories. In addition to the regular physical stress their bodies undergo, stressors like these can tip the balance towards the sympathetic nervous system and strain the body’s natural process of maintaining homeostasis.
This is especially true if pertinent treatment methods are not used to minimize sympathetic dominance and boost parasympathetic activity.
Evidence of Sympathetic Dominance by Heart Rate Variability
Heart rate variability (HRV) is a measure that indicates how much variation there is in your heartbeat intervals. The more consistent your heartbeat intervals within a given time frame (i.e. 60 seconds), the lower your HRV. The more varied the lengths of the intervals between your heartbeats, the higher your HRV.
Heart rate variability has been found to be a valid indicator of decreased parasympathetic response and/or increased sympathetic activity.
Researchers have found that parasympathetic activity or increased sympathetic activity will result in reduced HRV (Billman, 2013). Though previously thought to reflect only SNS activity, it is now widely accepted that changes in heart rate variability express variations in both the sympathetic and parasympathetic nervous systems (Haker et al., 2002)
In a study by James, Munson, Maldonado-Martin & Croix (2012), subjects participated in an intense exercise session (defined as running 800 meters six times at 95% VO2 max with a three-minute recovery period between each run). The subjects experienced an increased sympathetic influence on the heart and heart rate variability and a decreased parasympathetic response (James et al, 2012).
While the subjects in this example returned to baseline numbers after 24 hours, the study demonstrates that repeated, intense exercise stressed the subjects’ ability to engage parasympathetic responses and maintain homeostasis.
Acupuncture & the Parasympathetic System
When an athletes is under stress, such as during intense physical training, his or her autonomic nervous system can deviate, leading to the athlete’s becoming sympathetic-dominant. In this state, the athlete’s parasympathetic nervous system is impaired, causing the athlete to experience more difficult recovery. A full restoration of the natural balance between sympathetic and parasympathetic is the ideal solution.
In western medicine, there aren’t many safe maneuvers to enhance parasympathetic performance while suppressing sympathetic functions. Acupuncture, however, is one of the most effective tools for doing just this.
Various experiments have shown that acupuncture treatment does in fact modulate the autonomic nervous system, in addition to alleviating muscle tension, improving local blood flow, and increasing pain threshold (Barlas et al., 2000).
One example is a study of hypertensive rats, wherein direct stimulation of the sciatic nerve produced decreased sensitivity to pain and a profound decrease in arterial pressure and activity in the splanchnic sympathetic nerve. The change lasted for several hours following treatment (Yao et al. 1982).
Another study showed that magnitopuncture–a combination of acupuncture point pressing and magnetic treatment at Dazhui (DU14) and Neiguan (PC6) points–resulted in reduced sympathetic nerve activity and increased parasympathetic nerve activity at the end of a three-hour simulated driving task (Li et al.2003).
It was also reported that needle insertions in the vagal innervated area of the ear could reduce narcotic and alcohol withdrawal symptoms and the underlying physiological mechanisms–a result of increased parasympathetic nerve activity (Mendelson et al., 1978)
More data pointing to the fact that acupuncture can upregulate the parasympathetic nervous system found that acupuncture can induce release of endogenous (natural) opioids (Basbaum et al., 1984; Holaday et al.,1983; Terman et al.,1986; Watkins et al.,1986).
Downregulation of the sympathetic nervous system has also been implicated by research. For example, it was found that acupuncture can trigger a somato-autonomic reflex (Budgell et al.1996), which can in turn induce vasodilation–a parasympathetic response (Kaada et al.,1982). This can result in increased relaxation and calmness and reduced distress (Knardahl et al., 1998).
Acupuncture has been shown capable of significantly reducing heart rate, oxygen consumption (Lin et al.2009). This is thought to be a result of a reciprocal process: an increase in parasympathetic activity and a decrease in sympathetic activity (Nishijo et al. 1997).
There is still much to be learned about the relationship between acupuncture and the autonomic nervous system. However, there is significant enough evidence to show that acupuncture is a noteworthy treatment or adjunct treatment for the reversal of sympathetic dominance.
A Window of Opportunity
While stressors like physical exertion can create an an unhealthy state of sympathetic dominance, exercise recovery (handled correctly) grants a unique window of opportunity for the body to maximize the positive outcomes of its altered state.
Many of the processes that are responsible for the beneficial effects of exercise remain highly active during exercise recovery period. This window of time can be put to good use, with the correct acupuncture interventions, to improve the body’s adaptation to exercise training.
Research shows that a period of intense exercise increases insulin sensitivity, decreases blood lipid levels and reduces blood pressure after exercise, making the recovery period after exercise an ideal time for therapeutic acupuncture intervention (Halliwill et al., 2013).
These responses occur anywhere from two to three hours immediately following exercise (e.g., post-exercise hypotension), and they may last up to 48 hours or more (e.g., altered blood lipids).
Athletes have long taken advantage of this recovery period to improve training and athletic performance by strategically consuming macronutrients during recovery. This is because the metabolic changes associated with both endurance and resistance exercise and recovery may be enhanced with appropriate nutrient timing strategies.
Optimizing the intake of macronutrients using exercise recovery is a large area of research related to human performance that may translate to clinical populations and older adults (Esmarck et al., 2001). In the context of general populations, recovery from exercise may be used to mitigate the negative effects of some chronic diseases (Luttrell et al., 2015).
Evidence of Acupuncture and the Window of Opportunity
In the general population, this window of opportunity could be used to apply acupuncture interventions during a state of enhanced insulin sensitivity and blunted blood lipid levels. Ideally, these interventions could slow, or even reverse, the progression of chronic diseases, reducing the need for pharmacological interventions and improving quality of life.
Research presented in Effects of acupuncture on heart rate variability in normal subjects under fatigue and non-fatigue state by Zengyong Li, Chengtao Wang, Arthur F. T., Mak Daniel and H. K. Chow sheds more light on how acupuncture can work in tandem with this window of opportunity.
The goal of this study was to analyze the effects of acupuncture applied at Hegu (LI 4) points and Neiguan (PC6) points on heart rate variability in normal subjects under fatigue and non-fatigue states. Stimulations of the LI 4 points and PC 6 points created inverse effects to the stress and fatigue response.
In a fatigue state, stimulation of the LI 4 points and PC 6 points indicated a shift of sympathetic balance. In a non-fatigue state, the acupuncture adopted in this study apparently induced a significant increase in activity of both the sympathetic and the parasympathetic nerve system during the post-stimulation period in normal subjects, which was similar to the study by Haker et al. (2000), suggesting no modification in sympathetic balance in non-fatigue state.
This study concluded that acupuncture on the Neiguan (PC 6) and Hegu (LI 4) points seemed to enhance vagal (parasympathetic) activity and to suppress sympathetic activity. These effects on the autonomic nervous system were opposite to the stress and fatigue response, indicating that the acupuncture treatment was capable of reducing the effects of fatigue in a fatigue state.
These different effects of acupuncture on heart rate variability suggests that the modulating effect of acupuncture on HRV not only depends on the acupuncture points used, but that it was also connected to the functional state of the body (such as fatigue or non-fatigue) in normal subjects.
Since the temporary change in autonomic nervous system activity is associated with the functional state of human body, such as mental stress or fatigue (Pagani et al. 1989, 1994), it is reasonable to hypothesize that the effects of acupuncture on autonomic nervous system activity are associated with the functional state of the human body.
Conclusions
The research presented and analyzed in this essay shows that sports acupuncture can and should play a larger role in the field of recovery. While the treatment of injury is still a cornerstone of acupuncture for athletes, more attention must be paid to the recovery period and the window of opportunity. By focusing more on recovery, acupuncturists can help their clients to not only recover faster and more effectively, but also to improve their sports performance by utilizing key recovery states.
To help athletes properly recover and avoid overtraining it is important to:
- Monitor the intensity of athletes’ prescribed workouts; and
- Ensure that rest or active recovery days are part of the training program.
- Utilize acupuncture to help athletes switch out of workout induced sympathetic dominance and into parasympathetic state.
About the Author
 Willard Sheppy is a writer and healthcare practitioner who seamlessly melds scientific knowledge with practical applications in engaging and authoritative articles. He holds a Bachelor of Science in Environmental Science from Oregon State University and a Master’s in Acupuncture and Oriental Medicine from the distinguished Oregon College of Oriental Medicine.
Willard Sheppy is a writer and healthcare practitioner who seamlessly melds scientific knowledge with practical applications in engaging and authoritative articles. He holds a Bachelor of Science in Environmental Science from Oregon State University and a Master’s in Acupuncture and Oriental Medicine from the distinguished Oregon College of Oriental Medicine.
In his work, Willard skillfully combines his extensive educational background in scientific research with his practical experience as a healthcare practitioner. Willard balances his life with martial arts and cherished family adventures. As a father of three, he often leads his family on camping and hiking trips along the breathtaking Oregon coast.
Connect with Willard on LinkedIn at www.linkedin.com/in/valleyhealthclinic or learn more about his services at www.valleyhealthclinic.com. Embark on this journey towards holistic health with Willard guiding your way.
References
Akimoto, Takayuki, et al. “Acupuncture and responses of immunologic and endocrine markers during competition.” Medicine & Science in Sports & Exercise 35.8 (2003): 1296-1302.
Areta,J.L.,Burke,L.M.,Ross,M.L.,Camera,D.M.,West,D.W.D., Broad,E. M.,etal.(2013). Timing and distribution of protein ingestion during prolonged recovery from resistance exercise alters myofibrillar proteinsynthesis. J.Physiol. 591,2319–2331.doi:10.1113/jphysiol.2012.244897
BARLAS, P., J. ROBINSON, J. ALLEN, and G. D. BAXTER. Lack of effect of acupuncture upon signs and symptoms of delayed onset muscle soreness. Clin. Physiol. 20:449–456, 2000.
Basbaum AI, Fields HL. Endogenous pain control systems: Brainstem spinal pathways and endorphin circuitry. Annu Rev Neurosci 1984;7:309–338.
Billman GE (2013). “The LF/HF ratio does not accurately measure cardiac sympatho-vagal balance”. Frontiers in Physiology. 4: 26. doi:10.3389/fphys.2013.00026. PMC 3576706. PMID 23431279.
Braun,B.,Zimmermann,M.B.,and Kretchmer,N.(1995). Effects of exercise intensity on insulin sensitivity in women with non-insulin-dependent diabetes mellitus. J.Appl.Physiol. 78,300–306
Budgell B, Sato A. Modulations of autonomic functions by somatic nociceptive inputs. Prog Brain Res 1996;113:525–539.
Chao DM, Shen LL, Tjen-A-Looi S, Pitsillides KF, Li P, Longhurst JC (1999) Naloxone reverses inhibitory effect of electroacupuncture on sympathetic cardiovascular reflex responses. Am J Physiol Heart Circ Physiol 276:H2127–H2134
Crouse,S.F.,O’Brien,B.C.,Grandjean,P.W.,Lowe,R.C.,Rohack,J.J.,and Green,J.S.(1997). Effects of training and a single session of exercise on lipids and apolipoproteins in hypercholesterolemic men. J.Appl.Physiol. 83, 2019–2028.
Emhoff,C.A.,Barrett-O’Keefe,Z.,Padgett,R.C.,Hawn,J.A.,andHalliwill,J. R.(2011). Histamine-receptor blockade reduces blood flow but not muscle glucose uptake during post exercise recovery in humans. Exp.Physiol. 96, 664–673.doi:10.1113/expphysiol.2010.056150
Esmarck,B.,Andersen,J.L.,Olsen,S.,Richter,E.A.,Mizuno, M.,andKjaer, M.(2001). Timing of post exercise protein in take is important for muscle hypertrophy with resistance training in elderly humans. J.Physiol. 535, 301–311.doi:10.1111/j.1469-7793.2001.00301.x
Gleeson, M., W. A. McDonald, D.B. Pyne,, et al. Salivary IgA levels and infection risk in elite swimmers. Med. Sci. Sports Exerc. 31:67–73, 1999.
Grandjean,P.W.,Crouse,S.F.,and Rohack,J.J.(2000). Influence of cholesterol status on blood lipid and lipoprotein enzyme responses to aerobic exercise. J.Appl.Physiol. 89,472–480.
Haker E, Lundeberg T (1990) Acupuncture treatment in epicondylalgia: a comparative study of two acupuncture techniques. Clin J Pain 6:221–226
Haker E, Egekvist H, Bjerring P (2000) Effect of sensory stimulation (acupuncture) on sympathetic and parasympathetic activities in normal subjects. J Auton Nerv Syst 79:52–59
Halson,S.L.(2014).Monitoring training load to understand fatigue in athletes. SportsMed. 44,139–147.doi:10.1007/s40279-014-0253-z
Halliwill,J.R.,Buck,T.M.,Lacewell,A.N.,andRomero,S.A.(2013). Postexercise hypotension and sustained post exercise vasodilation: what happens after we exercise? Exp.Physiol. 98,7–18.doi:10.1113/expphysiol.2011.058065
Holaday JW. Cardiovascular effects of endogenous opiate systems. Annu Rev Pharmacol 1983;23:541–594.
Holloszy,J.O.(2005). Exercise-induced increase in muscleinsulin sensitivity. J.Appl.Physiol. 99,338–343.doi:10.1152/japplphysiol.00123.2005
James, D. V. B., Munson, S. C., Maldonado-Martin, S., & Croix, M. B. A. D. S. (2012). Heart rate variability: Effect of exercise intensity on postexercise response. Research Quarterly for Exercise and Sport, 83(4), 533-9.
Karvelas, B. R., M.D. Hoffman, A. I. Zeni. Acute effects of acupuncture on physiological and psychological responses to cycle ergometry. Arch. Phys. Med. Rehabil. 77:1256–1259, 1996.
Kenttä,G.,andHassmén,P.(1998). Overtraining and recovery: a conceptual model. SportsMed. 26,1–16.doi:10.2165/00007256-199826010-00001
Knardahl, S., M. Elam, B. Olausson,, and B. G. Wallin. Sympathetic nerve activity after acupuncture in humans. Pain 75:19– 25, 1998
Levenhagen,D.K.,Gresham,J.D.,Carlson,M.G.,Maron,D.J.,Borel, M.J.,and Flakoll,P.J.(2001). Post exercise nutrient intake timing in humans is critical to recovery of leg glucose and protein homeostasis. Am.J.Physiol.Endocrinol. Metab. 280,E982–E993.
Li ZY, Jiao K, Chen M, Wang CT (2003) Effect of magnitopuncture on sympathetic and parasympathetic activities in normal drivers during simulated driving. Eur J Appl Physiol 88: 404–410
Li-wen Guo, Ding-zhong Li (2002). Testing the effect of Haci Five Element Needle on human body using superconducting quantum interference device (in Chinese). Biomagnetism 1:3–5
Lin ZP, Lan LW, He TY, et al. Effects of acupuncture stimulation on recovery ability of male elite basketball athletes. Am J Chinese Med 2009;37:471–481
Luttrell, Meredith J., and John R. Halliwill. “Recovery from exercise: vulnerable state, window of opportunity, or crystal ball?.” Frontiers in physiology 6 (2015): 204.
Malik M, Camm AJ (1993) Components of heart-rate-variability – what they really mean and what we really measure. American Journal of Cardiology 72(11):821–822
Mendelson G (1978) Acupuncture and cholinergic suppression of the withdrawal symptoms: an hypothesis. Br J Addict 73:166– 170
Minett,G.M.,Duffield,R.,Billaut,F.,Cannon,J.,Portus,M.R., andMarino,F. E.(2014). Cold-water immersion decreases cerebral oxygenation but improves recovery after intermittent-sprint exercise in the heat. Scand.J.Med.Sci.Sports 24,656–666.doi:10.1111/sms.12060.
MIYAMOTO, T. Acupuncture treatment for muscle injury [in Japanese]. Jpn. J. Phys. Fitness Sports Med. 43:39–41, 1997.
Nishijo K, Mori H, Yosikawa K, Yazawa K (1997) Decreased heart rate by acupuncture stimulation in humans via facilitation of cardiac vagal activity and suppression of cardiac sympathetic nerve. Neurosci Lett 227(3):165–168
Pagani M, Furlan R, Pizzinelli P, Crivellaro W, Cerutti S, Malliani A (1989) Spectral analysis of R-R and arterial pressure variables to assess sympatho-vagal interaction during mental stress in humans. J Hypertension 7:S14–S15
Pagani M, Lucini D, Mela GS, Langewitz W, Malliani A (1994) Sympathetic overactivity in subjects complaining of unexplained fatigue. Clin Sci 87:655– 661
Pedersen, B. K., and D. C. Nieman. Exercise immunology: integration and regulation. Immunol. Today 19:204–206, 1998.
Peltham, T. W., L. E. Holt, and R. Stalker. Acupuncture in human performance. J. Strength Cond. Res. 15:266–271, 2001.
Terman GW, Liebeskind JC. Relation of stress-induced analgesia to stimulation-produced analgesia. Ann NY Acad Sci 1986;467:300–308.
Wang JD, Kuo TBJ, Yang CCH (2002) An alternative method to enhance vagal activities and suppress sympathetic activities in humans. Auton Neurosci-Basic Clin 100(1–2):90–95
Watkins LR, Mayer DJ. Multiple endogenous opiate and nonopiate analgesia systems: Evidence of their existence and clinical implications. Ann N Y Acad Sci 1986;467:273–299.
Yao T, Andersson S, Thore P (1982) Long-lasting cardiovascular depression induced by acupuncture-like stimulation of the sciatic nerve in unanaesthetized spontaneously hypertensive rats. Brain Res 240:77–85

 Willard Sheppy is a writer and healthcare practitioner who seamlessly melds scientific knowledge with practical applications in engaging and authoritative articles. He holds a Bachelor of Science in Environmental Science from Oregon State University and a Master’s in Acupuncture and Oriental Medicine from the distinguished Oregon College of Oriental Medicine.
Willard Sheppy is a writer and healthcare practitioner who seamlessly melds scientific knowledge with practical applications in engaging and authoritative articles. He holds a Bachelor of Science in Environmental Science from Oregon State University and a Master’s in Acupuncture and Oriental Medicine from the distinguished Oregon College of Oriental Medicine.